Is Acne an Inflammatory Skin Condition?
Yes, acne is now widely recognised as a chronic inflammatory skin condition, rather than simply a surface-level skin problem. Many forms of acne - including inflammatory acne, adult acne, hormonal acne, and cystic acne - are driven by ongoing, low-grade inflammation within the body.
At Fitzwilliam Food Test, acne is viewed as a systemic condition with clear links to immune function, gut health, and inflammation.
Martin Healy explains in this video:
Martin Healy - Fitzwilliam Food Test Clinic
The Root Cause of Inflammatory Acne
In many individuals, chronic low-grade inflammation is continuously activated within the immune system. This persistent inflammatory response can directly affect the sebaceous (oil) glands in the skin.
When these glands become inflamed, they begin to overproduce sebum. Excess oil creates the ideal environment for the overgrowth of Cutibacterium acnes (acne-causing bacteria).
It is the combined effect of:
Systemic inflammation
Excessive sebum production
Acne-causing bacteria
that leads to inflamed acne lesions, including papules, pustules, nodules, and cysts.
Hormonal Imbalance, Inflammation & Acne
Hormonal imbalance is commonly associated with acne, particularly adult female acne. However, conditions such as polycystic ovary syndrome (PCOS) and endometriosis are also now understood to be inflammatory conditions, closely linked to immune dysfunction.
Chronic inflammation interferes with normal hormonal signalling, infiltrating glandular tissue and causing it to malfunction. This explains why addressing hormones alone often fails to fully resolve acne if inflammation remains untreated.
Why Antibiotics Don’t Address the Root Cause of Acne
Conventional acne treatment frequently relies on antibiotics to reduce skin bacteria. While this can temporarily suppress symptoms, it does not address the underlying inflammatory drivers of acne.
This is why acne often returns once antibiotics are discontinued - and why repeated courses are commonly prescribed.
Gut Health, Immune Function & Acne Inflammation
Inflammation originates in the immune system - and approximately 70–80% of immune tissue is located in the gut.
When certain foods are poorly digested (food sensitivities), they can ferment in the gut, becoming toxic and irritating to the immune system. This immune activation is a major source of systemic inflammation, which can manifest in the skin as acne.
At Fitzwilliam Food Test, identifying food sensitivities and measuring and monitoring gut-driven inflammation is a key step in addressing the root cause of inflammatory skin conditions, including acne.
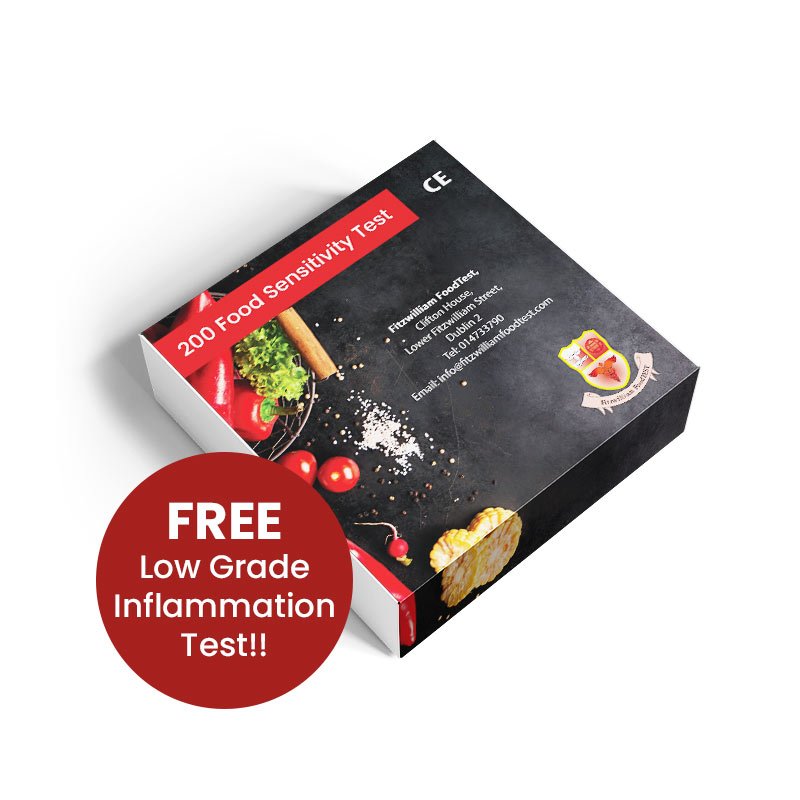
200 Food Sensitivity Test
Commonly referred to as Food Test 200. This test checks your IgG antibody levels to 200 of the most common foods typically associated with food intolerance. This information can be used to guide your food elimination diet.
*Please note: The “Low Grade Inflammation Test” comes FREE of charge with the 200 test.
Acne & Food Sensitivities: Frequently Asked Questions
Can food sensitivities cause acne?
Yes. Food sensitivities can contribute to acne by triggering chronic, low-grade inflammation in the immune system. Unlike food allergies, food sensitivities often cause delayed reactions that may appear hours or days later. This ongoing immune activation can manifest in the skin as inflammatory acne, cystic acne, or adult acne.
What is the link between inflammation and acne?
Acne is now understood to be a chronic inflammatory skin condition. Systemic inflammation can stimulate the sebaceous glands to overproduce oil, disrupt skin barrier function, and encourage the growth of acne-causing bacteria (Cutibacterium acnes). When inflammation remains unaddressed, acne is more likely to persist or recur.
Can gut health affect acne?
Yes. Gut health plays a central role in skin health. Around 70–80% of the immune system is located in the gut. When digestion is compromised or food sensitivities are present, immune activation in the gut can lead to systemic inflammation, which may present as acne and other inflammatory skin conditions.
Why does acne return after antibiotic treatment?
Antibiotics can temporarily reduce acne by suppressing bacteria on the skin. However, they do not address the underlying causes of acne, such as inflammation, immune dysfunction, or food sensitivities. This is why acne often returns once antibiotics are stopped and why repeated courses are frequently required.
Are food sensitivities the same as food allergies?
No. Food allergies cause immediate reactions involving IgE antibodies, while food sensitivities cause delayed immune responses involving different pathways. Food sensitivities are often harder to identify but can lead to chronic inflammation, digestive symptoms, fatigue, joint pain, and inflammatory skin conditions like acne.
Can hormonal acne be linked to food sensitivities?
Yes. Hormonal acne is closely associated with inflammation. Food sensitivities can worsen hormonal imbalance by increasing inflammatory load and disrupting gut–hormone communication. Conditions such as PCOS and endometriosis, which are often linked with acne, are also associated with chronic inflammation.
How long does it take to see skin improvement after removing trigger foods?
Skin improvement timelines vary, but many people notice changes within 2-4 weeks after removing identified trigger foods and reducing inflammation. Long-standing or severe acne may take longer to fully resolve, depending on immune and gut health.
Is food sensitivity testing suitable for adult acne?
Yes. Adult acne, particularly acne that is persistent, cyclical, or resistant to conventional treatment, is often associated with inflammation and immune activation. Food sensitivity testing can be especially helpful in identifying hidden triggers in adult acne cases.
How does Fitzwilliam Food Test approach acne differently?
At Fitzwilliam Food Test, acne is approached as a systemic inflammatory condition, not just a skin issue. By identifying food sensitivities, immune triggers, and sources of chronic inflammation, the focus is on addressing the root cause of acne, rather than managing symptoms alone.